Referral information and fertility facts
For fertile women aged 35 years or younger, about
- 60% will have conceived after 6 months
- 80% after 12 months, and
- 95% after 24 months
- a normal fertility rate is achieved with intercourse every couple of days during the most fertile time of the menstrual cycle
- smoking halves pregnancy rates
- being overweight or underweight can affect ovulation and reduce response to fertility drugs
- high alcohol or caffeine intake may reduce fertility.
Check:
- female rubella status
- taking folic acid
- weight gain if anovulatory
- occupational history
- drug history
- cervical smear history
Advice:
- weight loss if BMI more than 28
- stop smoking
- minimal alcohol and caffeine intake
- regular intercourse (2-3 times a week)
Wondering what to order before referring your patient to FA?
Investigation
- progesterone 6 - 8 days before menses
- FSH and estrad. day 2 - 4 of cycle
- semen analysis – repeat in 4 - 6 weeks unless totally normal
- prolactin and thyroid function ONLY if irregular cycles
- AMH Test – to check ovarian reserve
Further investigation for public referral:
- laparoscopy if duration more than 1 year, unless severe ovulation or severe sperm factor
Refer when:
- no pregnancy and Biological Clock indicates status in red or orange region, OR
- any abnormal results on investigation
Early referral if:
- extreme anxiety about fertility
- woman aged 35 years or older
- irregular cycles or anovulation
- severe sperm factor
- previous abdo/pelvic/urogenital surgery
- previous STD
- two or more consecutive miscarriages
- abnormal pelvic/genital examination (woman or man)
- family history of menopause between 40-45 years or earlier
- significant systemic illness
- genetic conditions (e.g. cystic fibrosis, muscular dystrophy or Huntington’s disease)
Immediate referral before starting cancer treatment
- sperm, eggs, ovarian tissue or testicular tissue stored before starting cancer treatment.
- access to publicly-funded fertility preservation for the retrieval, freezing and long-term storage of gametes, (specifically sperm and eggs), is available for people whose fertility will be permanently impaired by publicly-funded treatment for medical conditions, such as by cancer treatment." [Service Coverage Schedule 2016/17.]
How do I refer?
You may refer patients to the specialist of your choice in a number of ways:
- by letter
- via Healthlink. Our referral codes are: Auckland - fertaakl; Wellington - fertawtn; Hamilton - fertaham; Christchurch & Dunedin– fertachr
- e-refer live via Specialists & Referrals (SR)
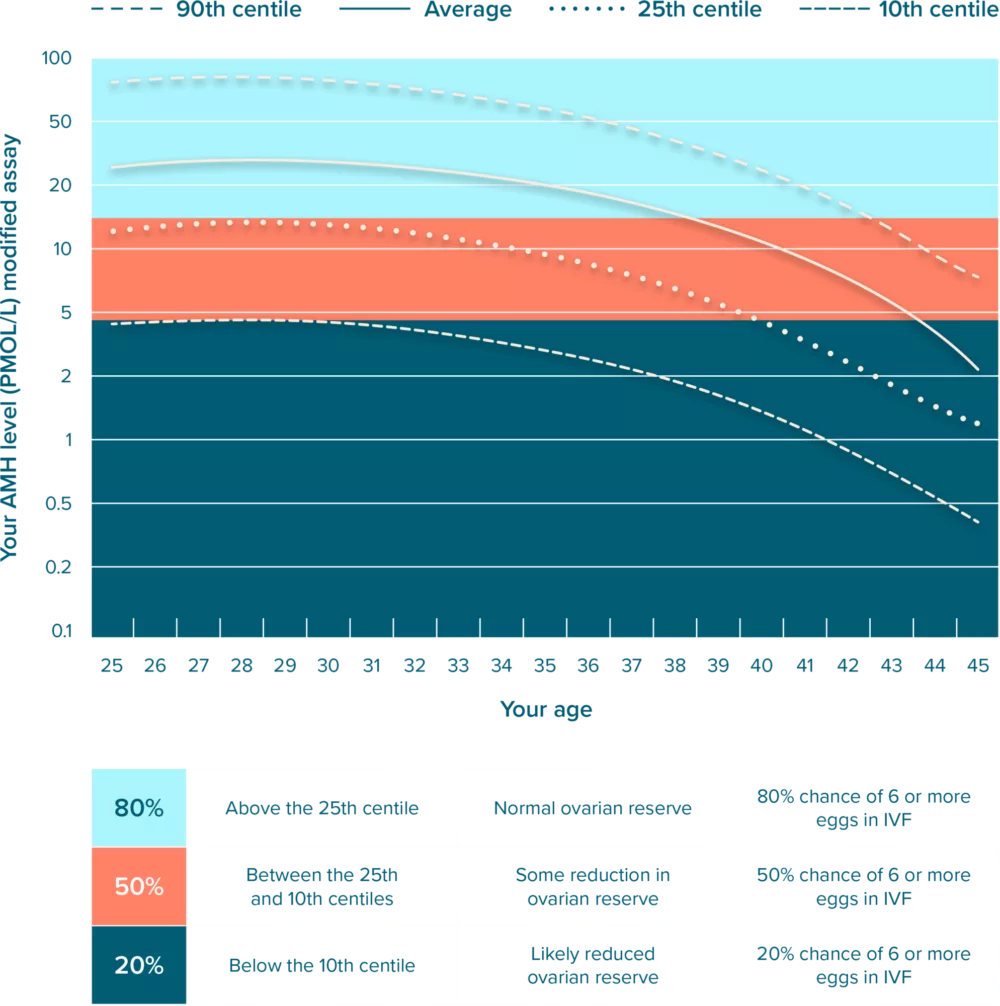
Anti-Müllerian Hormone (AMH) test
For most women, age best predicts the chance of conception each month. However, despite having regular menstrual cycles and normal periods, about 10% of women lose their fertility sooner than expected. These women should think about having a family in their 20’s or very early 30’s. The AMH test is considered the best test currently available to estimate ovarian reserve.
- This test is more convenient and less expensive than alternative tests like Egg Check, because it uses a simple blood test rather than ultrasound scanning, and can be done at any time in the menstrual cycle.
- It can help predict how many eggs you are likely to obtain in an IVF cycle.
- It may also identify women who may undergo early menopause, and therefore who may lose their fertility earlier than average.
- Although an AMH test can help pick up those who might lose their fertility more quickly, it cannot show who is more fertile than average, nor does it predict ovarian reserve in women with Polycystic Ovaries (PCO).
- It is available from all Fertility Associates clinics.
Important points
Please remember that age is still a very important factor for fertility. The AMH tests can suggest when a woman might have lower fertility than expected for her age. However, there is no evidence that ‘good’ AMH results mean that women have a higher fertility than expected for their age.
- We strongly recommend all women start their family well before 40 years of age.
- A normal AMH result does not exclude other possible causes of reduced fertility.
Graph of Anti-Müllerian Hormone (AMH) levels
The graph shows the average AMH level for women without fertility problems according to age (the dark line) and the 10th, 25th and 75th centiles for this group of women.
More helpful information
Hormones explained (FSH, Progesterone)
FSH, E2 & Progesterone
Day 2 FSH and E2 Measurement
This is sometimes abbreviated to “basal FSH measurement” but would be better described as “FSH measurement when the E2 is basal” (ie at the time of a period).
What is FSH?
FSH is Follicle Stimulating Hormone, and it is produced by the brain, (via the pituitary gland), to stimulate follicles in the ovary to grow. When the brain realises that there is low E2 around, (ie at the time of a period), and a further group of follicles should be recruited to start another cycle, the blood level of FSH rises, but generally to not more than 9iu/l. If more FSH than 9iu/l is produced at the time of a period, the brain has somehow realised that to stimulate follicles to grow, more FSH is required than is normal – and the usual reasons for this are that the number of follicles in the ovary is low, or there is some problem within the follicles that the FSH needs to overcome to stimulate another menstrual cycle.
What is E2?
E2 is the steroid hormone that is produced by the cells lining the ovarian follicles in response to FSH, and the very high levels of E2 within the leading follicle nourish and mature the egg. Some E2 reaches the blood to cause the lining of the uterus to grow, the secretion of ovulatory cervical mucus, and to provide feedback to the brain and pituitary that another cohort of follicles has been recruited and is growing. The level of FSH then falls due to negative feedback by E2.
Why measure around Day 2?
At this time, E2 is at its lowest so FSH should be at its highest. If the E2 level on Day 2 is > 200pmol/l, then follicle growth will have already started, and the measurement of the FSH is not reliable because the raised E2 will have already started to suppress the FSH level. This commonly happens in older women. From a functional point of view, early follicle growth may mean the endometrium does not have enough time to develop before ovulation occurs, leading to asynchronicity between the egg and the endometrium, hence a reduced chance of implantation.
Possible interpretation of results are:
- FSH < 9 iu/L; E2 < 200pmol/l = normal basal follicle function, and normal amount of FSH being produced to stimulate the ovarian follicles
- FSH >9 iu/l; E2 < 200 pmol/l = brain responds to low ovarian reserve by producing more FSH to try to recruit a follicle, ie. the brain is upping the production of its own fertility drug in recognition that there is something not right with follicle development.
- FSH < 9 iu/l; E2 > 250 pmol/l = ovary is racing ahead in follicle development, and correct interpretation of the FSH result is not possible because the E2 level is not basal.
- FSH > 9 iu/l; E2> 250 pmol/l = ovary is racing ahead of follicle development, and although interpretation of the FSH result is compromised by raised estra., it is likely that were the estra. to be basal, (ie< 200pmol/l), the FSH would be even higher.
Day 21 Progesterone Measurement
The corpus luteum is the gland formed in the ovary from the ovulated follicle(s). It makes progesterone and E2 that is secreted in the blood and causes the lining of the uterus to become secretory. Blood level of progesterone in the middle of the luteal phase > 30nmol/l suggest that the endometrial effect of the progesterone is likely to be sufficient to assist an embryo implanting in the uterus. This progesterone in the blood also feeds back to the pituitary to ensure that little FSH is produced. There is no value in measuring the hormones FSH, LH and E2 at the same time as a Day 21 progesterone because their interpretation is not of any value if the progesterone is raised, as it should be in the mid-luteal phase.
Why Day 21?
This day is chosen on the assumption that a woman is having a 26-30 day cycle, and luteal phase is normal and lasts about 10-14 days after ovulation. Thus, assuming ovulation is between days 12-16 , day 21 is the middle of the luteal phase when the production of progesterone from the corpus luteum gland peaks in an ovulatory cycle, (and if there was then pregnancy, the HCG would prevent the corpus luteum from then dying and it would produce even more progesterone). If ovulation has occurred later than days 12-16, then the progesterone check would be better done a few days later so as to strike the middle of the luteal phase. Conversely, if ovulation has occurred earlier than day 12, an earlier progesterone test at about day 18 is required.
Progesterone levels should be interpreted with respect to the number of days before the onset of the next period. Luteal function, (and hence ovulation), cannot be assumed if the period starts < 5 days later or > 9 days after the blood test.
Possible interpretation of results assuming the test is properly timed are:
- Progesterone > 30nmol/l – ovulation has occurred and the corpus luteum is producing sufficient progesterone to induce adequate secretory changes in the endometrium to assist implantation.
- Progesterone 3-30 nmol/l – ovulation has occurred > 10 days ago or < 5 days ago, or if ovulation did occurr 5-10 days ago, the level is probably not adequate to sustain endometrial growth for satisfactory implantation.
- Progesterone >120 nmol/l – two or more follicles have been recruited
- Progesterone < 3nmol/l – no ovulation in previous 14 days.




